[DIGEST: The Scientist, Technology Review, Inverse, Science]
Can the underlying cause of neurological disorders like Alzheimer’s and Parkinson’s be traced back to our own immune system?
Diseases like Alzheimer’s are attributed to a buildup of proteins in the brain that form plaques and tangles, leading to the loss of brain connections. But scientist Beth Stevens theorizes that the underlying cause of degenerative neural conditions takes place well before the buildup of proteins. Stevens, along with researchers from MIT and Harvard, believe that aberrant synaptic elimination is to blame.

Our brains are constantly undergoing a process in which weak or damaged synapses are cleared out or “pruned” to keep everything running smoothly. The cells responsible for pruning faulty synapses are called microglia, and until recently they’ve been largely overlooked by the scientific community.
Microglia were previously thought to be nothing more than a sort of neurological janitorial service. When brain cells are damaged, microglia gobble up the injured bits while another type of glia called astrocytes creates scar tissue. The process is known as gliosis.
Stevens’ mentor, Stanford biologist Ben Barres, has been studying microglia for decades. “It was just really fascinating,” he says. “The great mystery was: what is the point of
this gliosis? Is it good? Is it bad? Is it driving the disease process, or is it trying to repair the injured brain?”
Barres found that a protein called C1q that marks injured or unused cells for elimination triggers the pruning process. To keep the flow of neural transmissions efficient, the brain needs only the synapses that are actually in use, so the C1q protein is integral to healthy brain development. But in fully-developed, healthy neurons, the C1q protein is virtually absent.
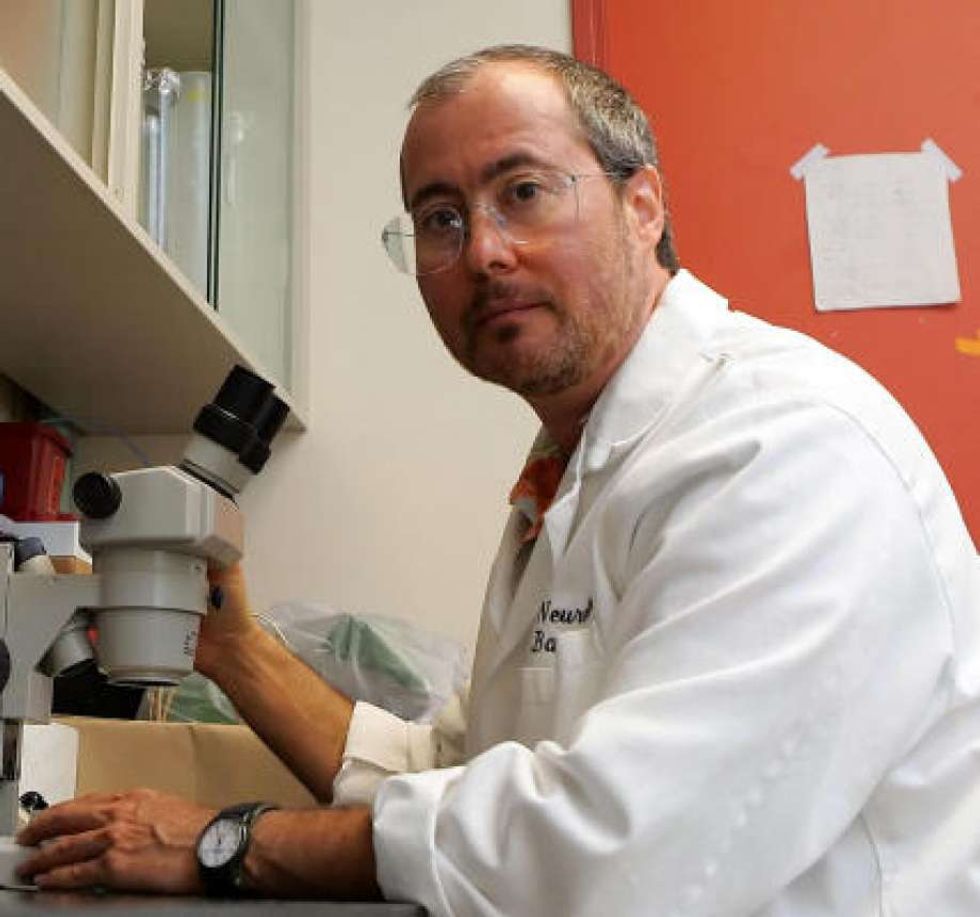
Barres and Stevens conducted research on mice bred to develop neurological disorders. They found that not only was the C1q protein present in adult cells, but it also appeared before any other detectable sign of the disease. It was evident even before cells started dying.
Steven McCarroll, Ph.D. led a study identifying a similar protein, C4, that is activated in schizophrenic brains.
“I think the implication of that is they could be lifelong diseases,” says Barres. “The disease process could be going on for decades and the brain is just compensating, rewiring, making
new synapses.”
In January, Stevens, McCarroll and a team at the Broad Institute of MIT and Harvard published a paper showing that aberrant microglia can cause or contribute to massive cell loss leading to cognitive defects like schizophrenia.

But what does that mean for treatment? Could devastating conditions like Alzheimer’s, schizophrenia and Parkinson’s be halted by the targeted suppression of synapse proteins?
Barres founded a company called Annexon Biosciences to develop a drug that could block C1q. Last week, Barres, Stevens and their colleagues published a paper showing that the drug was able to prevent mice bred to develop Alzheimer’s from showing signs of the disease.
The company hopes to start human trials in the next two years. “We’re a ways away from a cure,” says Stevens. “But we definitely have a path forward.”
 SECONDNEXUS
SECONDNEXUS percolately
percolately georgetakei
georgetakei comicsands
comicsands George's Reads
George's Reads